In part 1 we reviewed how antibiotics work, part 2 what biofilms are and their role in antibiotic resistance. In part 3 we will review:
- When antibiotics are needed and when they aren’t appropriate
- Distinguish between an allergic reaction to an antibiotic and the symptoms the infection is treating
When antibiotics are needed and when they aren’t appropriate
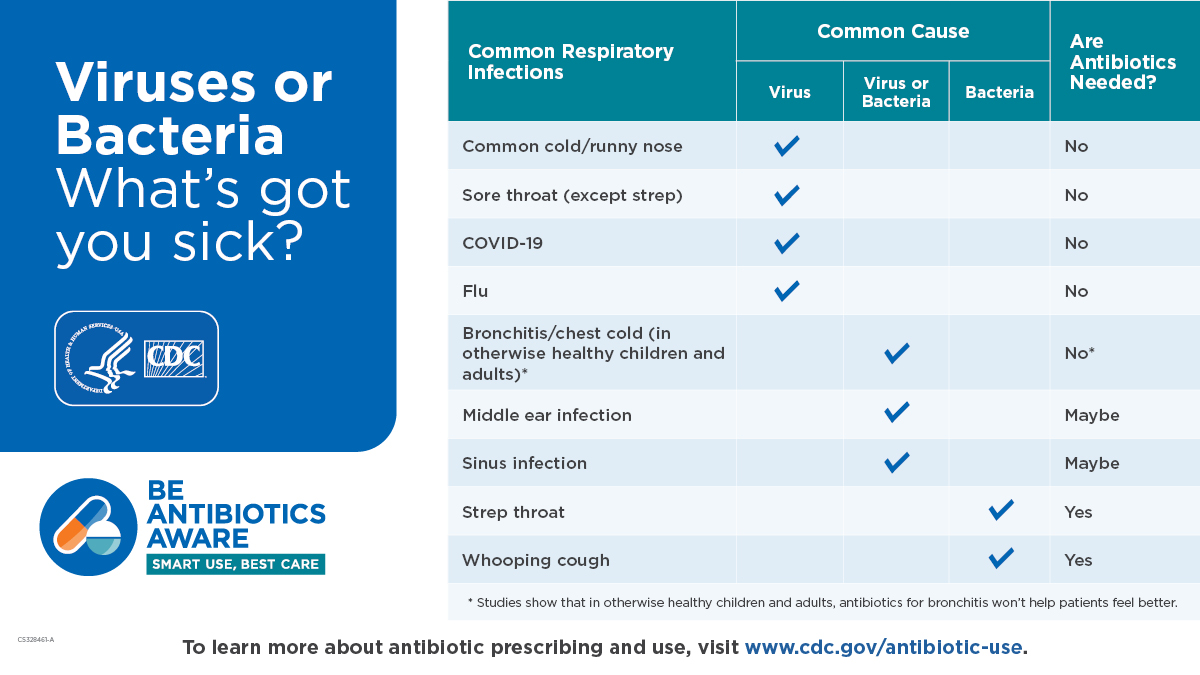
Antibiotic stewardship is one of the most pressing health issues of our time. As pathogens mutate and evade antibiotic therapy, we are forced to use more potent antibiotics. The use of antibiotics when not necessary is leading to devastating consequences. Antibiotic resistance, AKA antimicrobial resistance happens when germs like bacteria or fungi no longer respond to the drugs designed to kill them. According to the CDC: “About 47 million antibiotic courses are prescribed for infections that don’t need antibiotics, like colds and the flu, in U.S. doctors’ offices and emergency departments each year. That’s about 28% of all antibiotics prescribed in these settings.”
In the U.S., more than 2.8 million antimicrobial-resistant infections occur each year. A list of the antimicrobial resistant infections are listed on the CDC website. Some are familiar to the general population such as MRSA- Methicillin resistant Staphylococcus aureus, and VRE- Vancomycin resistant Enterococci. Some not so familiar-Drug resistant Candida and Carbapenem-resistant Acinetobacter for example. A full list of CDCs watchlist can be found here.
Antibiotics are indicated when:
A bacteria or fungal infection has taken over the body, either systemically (in the body) or topically-skin and tissues. Entry points can be a break in the skin, respiratory inhalation, eyes. Ears, mouth, urogenital route, or ingestion. They are not needed in all cases, sometimes our body can fight off the infection. If you own a Jase case check with your care provider when in question. They are not appropriate for viral illnesses such as colds, flu, covid, etc. Sometimes a viral infection will lower the body’s immune defenses allowing an opportunistic bacterial or fungal infection to take over as in the case of a viral pneumonia to bacterial pneumonia. At that point an antibiotic may be needed.
Distinguish between an allergic reaction to an antibiotic and the symptoms the infection is treating
Penicillin, the most commonly reported antibiotic allergy is less common than believed to be.
This is a great you tube video on penicillin allergies
According to the CDC: Although 10% of the population in the U.S. reports a penicillin allergy, less than 1% of the population is truly penicillin allergic.
The difference between a side effect and allergy
Side effects to antibiotics
- Nausea, vomiting
- Diarrhea
- Mild rash
- Photosensitivity
- Vaginal yeast infection
- Thrush
Allergic reaction to antibiotics- Seek medical care immediately
- Severe rash/hives
- Peeling skin
- Anaphylactic reactions such as:
- Respiratory distress/wheezing
- Throat closing/tightness
- Brooke Lounsbury
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Antibiotic Shortage Leads to Increase in Syphilis Cases
According to the CDC: “Reported syphilis cases increased 80% in the United States between 2018 and 2022, (from 115,000 to more than 207,000), compounding a decades-long upward trend. If untreated, syphilis can seriously damage the heart and brain and can cause...
Ivermectin for Scabies- and More
Discovered in the late 1970s and approved as a commercial product for animal health in 1981, ivermectin, an antiparasitic drug was initially used by veterinarians to treat mite and heartworm infections. In 1988, ivermectin was approved to treat Onchocerciasis (known...
How Should I Store My Jase Case and Add-ons?
You recently made the proactive decision to purchase the Jase Case and some add-ons. This investment is a hedge against interrupted medication supplies due to natural disasters, travel to medically underserved regions of the world, and world events leading to extended...