In part 1 the history of antibiotics and how they work was reviewed. This week we will look at
- The role of biofilms in bacteria and why these present a challenge to our modern-day arsenal of antibiotics
- Antibiotic resistance challenges
The role of biofilms in bacteria and why these present a challenge to our modern-day arsenal of antibiotics
What are biofilms?
It wasn’t until the 1970s that biofilms were found to play a role in bacterial infections in cystic fibrosis patients. Bacterial biofilms are clusters of bacteria that are attached to a surface and/or to each other and embedded in a self-produced matrix of fibrin like proteins or polysaccharides.
The matrix attaches to a surface and manufactures a slimy substance that offers protection that live within the biofilm. This substance is called the Extracellular Matrix (ECM)
The ECM matrix includes proteins, polysaccharides, glycolipids, glycoproteins, and DNA. There can be more than one bacterium or microbe in the matrix which can transfer genetic material between them. This promotes adaptation of the microbes.
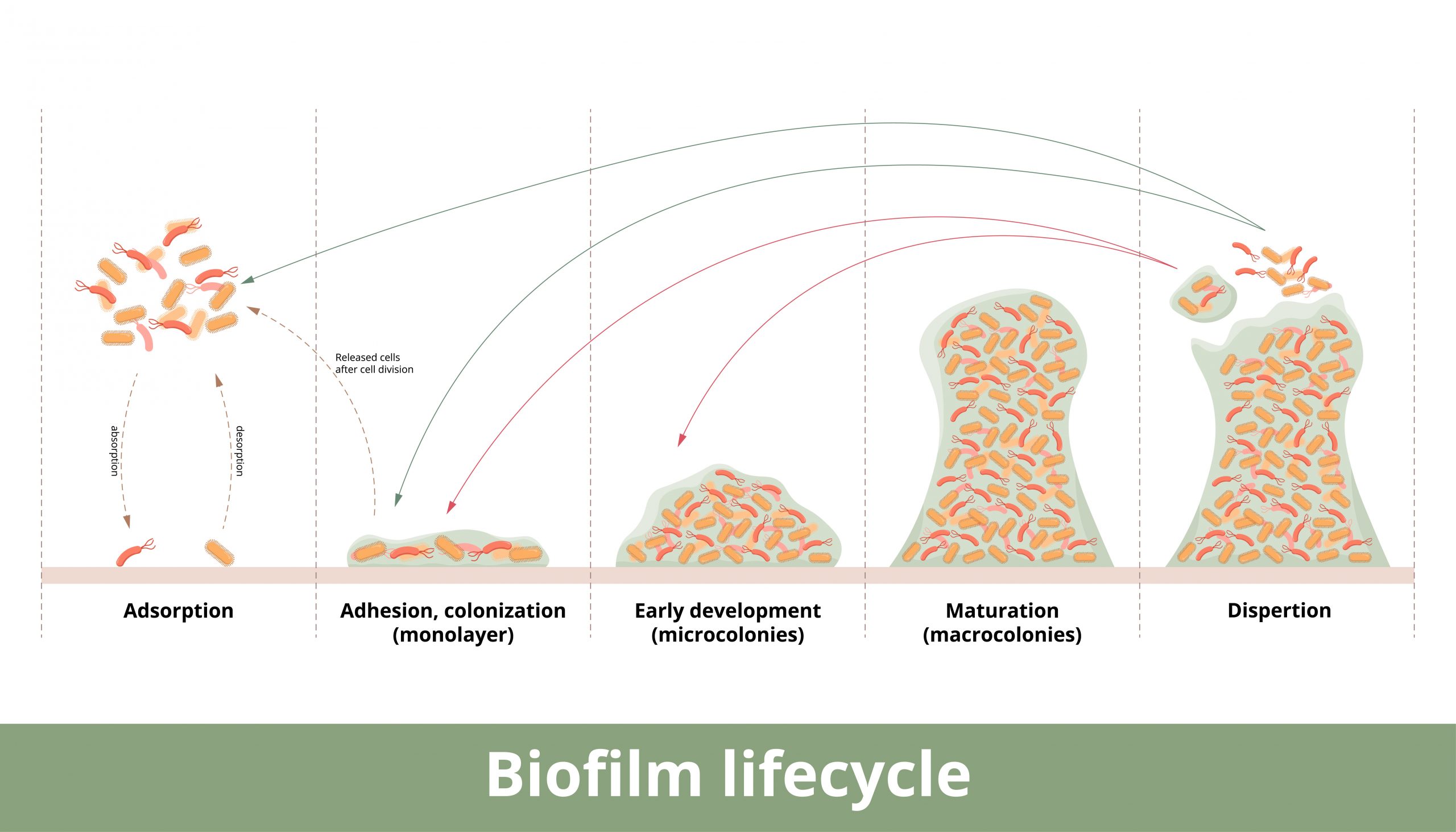
For instance, Staphylococcus aureus can form biofilm in four different ways- from polysaccharides to protein/DNA to fibrin to amyloid biofilms. The biofilm protects the bacterium from penetration of any invasive substances that would kill it. This can make the bacteria highly resistant to antibiotics where it can hide within this matrix and can re emerge after antibiotic therapy to reinfect the host.
The National Institutes of Health (NIH) revealed that among all microbial and chronic infections, 65% and 80%, respectively, are associated with biofilm formation. Of note is that biofilms can form on living and nonliving surfaces such as indwelling catheters, implanted medical devices, and protheses.
Common bacteria associated with Biofilm
Staphylococcus aureus
The most common infection associated with implants and medical devices. These devices are very susceptible to biofilm infection. Removal of the implant or device can help bring the infection under control in some instances, however some bacteria are usually dislodged upon removal and take up residence in other parts of the body.
Pseudomonas aeruginosa
According to PubMed “Pseudomonas aeruginosa is an opportunistic human pathogen causing devastating acute and chronic infections in individuals with compromised immune systems. Its highly notorious persistence in clinical settings is attributed to its ability to form antibiotic-resistant biofilms.” It is found in both indwelling medical devices, catheters, ventilators and in humans.
P aeruginosa is also a major cause of hospital acquired infections, ranging from ventilator associated pneumonia to cystic fibrosis patients succumbing to this infection and diabetics with non-healing ulcers.
Escherichia coli
A major cause of urinary tract infections and can be difficult to eradicate.
Biofilm-associated diseases of different body systems and their affected organs.
Some of the more common biofilm associated diseases include:
- Otitis media- ear infection
- Cardiac valve-Infective endocarditis
- Arteries- Atherosclerosis
- Salivary glands- Salivary duct stones
- Gastrointestinal tract- Inflammatory bowel disease and colorectal cancer
- Skin and underlying tissue- Wound infections
- Vagina- Bacterial vaginosis
- Uterus and fallopian tubes- Chronic endometritis
- Mamary glands- Mastitis
- Nasal cavity and paranasal sinuses- Chronic rhinosinusitis
- Throat, tonsils, adenoids, larynx and vocal cords- Pharyngitis and laryngitis
- Respiratory- Upper and lower airways- Cystic fibrosis, pseudomonas pneumonia
- Mouth- dental caries
Antibiotic resistance challenges
As we enter a world where antibiotic resistance becomes more commonplace there are a few measures we can take to help alleviate this.
The 4 Rs of home antibiotic therapy:
- Right person- don’t share antibiotics
- Right route- by mouth, injection or topical
- Right time- and how often to take
- Right dose- don’t skip or save antibiotics, finish entire course of therapy
Research points to taking low doses of or not completing antibiotic therapy can cause antibiotic resistance- the pathogenic (disease causing) bacteria aren’t all the way eradicated. This, in turn allows the bacteria time to mutate and develop resistance to the antibiotic.
- Use antibiotics appropriately
Antibiotics treat bacteria and, in some cases, parasitic and fungal infections. They do not treat viruses. Overuse and not used appropriately has led to antibiotic resistance. This in turn forces the practitioner to use stronger antibiotics with more side effects.
- Biofilm disruptors
Combination drug therapies are sometimes used to combat biofilm.
There is a growing body of evidence that some spices and foods can act as biofilm disruptors, allowing antibiotics to reach the pathogenic bacteria. One is turmeric. Others include oil of oregano and cranberry, used in urinary tract infections.
- Brooke Lounsbury
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Antibiotic Shortage Leads to Increase in Syphilis Cases
According to the CDC: “Reported syphilis cases increased 80% in the United States between 2018 and 2022, (from 115,000 to more than 207,000), compounding a decades-long upward trend. If untreated, syphilis can seriously damage the heart and brain and can cause...
Ivermectin for Scabies- and More
Discovered in the late 1970s and approved as a commercial product for animal health in 1981, ivermectin, an antiparasitic drug was initially used by veterinarians to treat mite and heartworm infections. In 1988, ivermectin was approved to treat Onchocerciasis (known...
How Should I Store My Jase Case and Add-ons?
You recently made the proactive decision to purchase the Jase Case and some add-ons. This investment is a hedge against interrupted medication supplies due to natural disasters, travel to medically underserved regions of the world, and world events leading to extended...