Resiliency: an ability to recover from or adjust easily to misfortune or change. Change or misfortune can be physical, mental, or emotional. Our ability to recover and thrive from change or misfortune reflects on how resilient we are. The past several years- pandemic,...
Silent Pandemic – Antibiotic Resistance

A dire warning from health leaders across the world are calling the silent pandemic- antimicrobial resistant (AMR) infections. According to the World Health Organization AMR is one of the top ten leading global threats to health facing humanity in the world.
CDC estimates about 47 million antibiotic courses are prescribed for infections that don’t need antibiotics, like colds and the flu, each year. That adds up to approximately 28% of all antibiotics prescribed. In addition, A study published in the Lancet found that antimicrobial resistance was the direct cause of 1.27 million deaths worldwide.
An ever-increasing number of bacteria, fungi and parasites are becoming resistant to commonly prescribed antibiotics, with some resistant to many different antibiotics. In some cases, antibiotics are not effective, leading to impossible to treat infections. This is a chilling scenario we are facing.
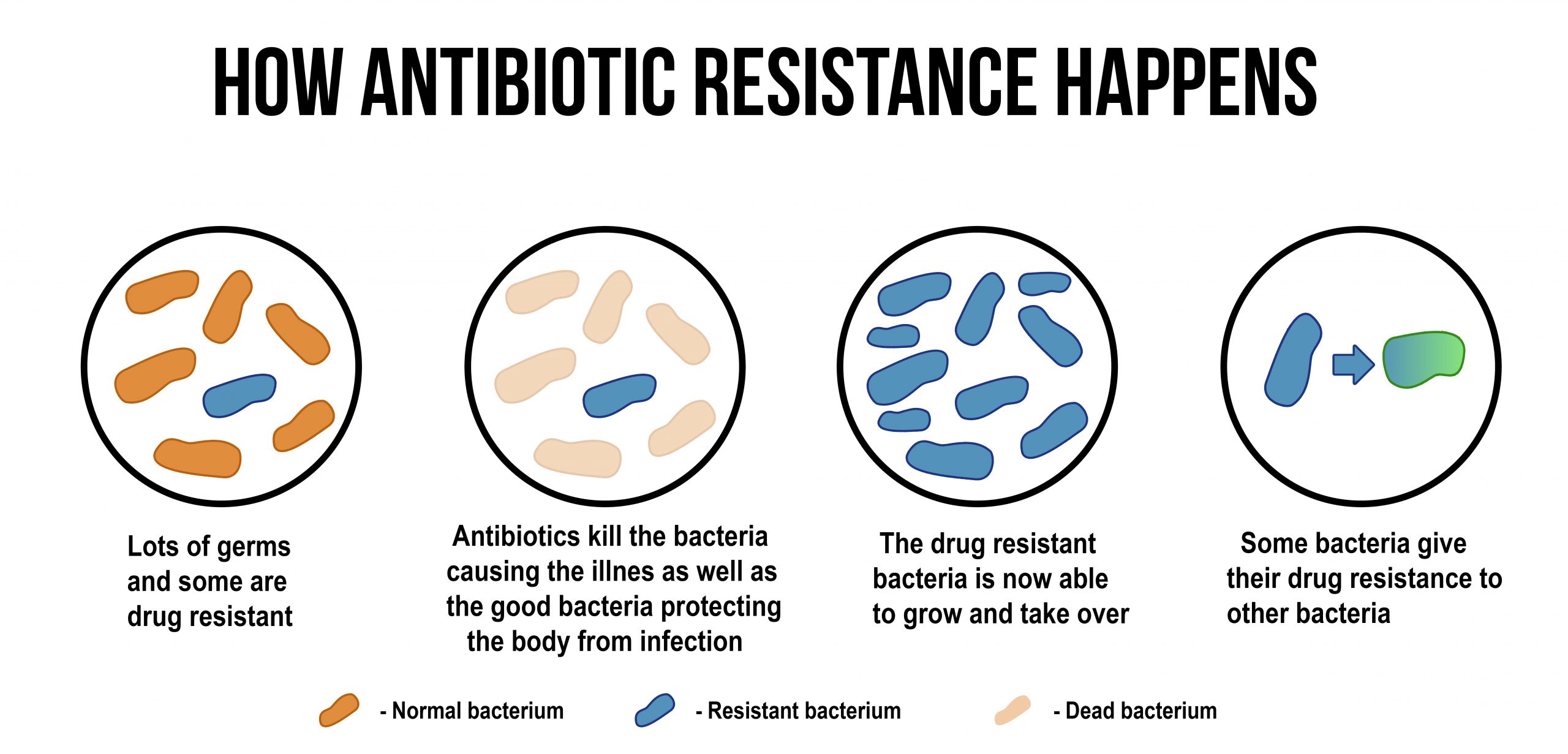
Antibiotic resistance (AMR) occurs through either genetic mutation or by acquiring resistance genes- where the antibiotic resistance genes are transferred to the next generation.
Some of the most widespread and common examples include:
- methicillin-resistant Staphylococcus aureus (MRSA) (The most common)
- vancomycin-resistant Enterococcus (VRE)
- multi-drug-resistant Mycobacterium tuberculosis (MDR-TB)
- carbapenem-resistant Enterobacteriaceae (CRE) gut bacteria
Broad spectrum antibiotics- The good and the bad
Broad spectrum antibiotics are being used in more and more AMR cases. These are antibiotics that act on the two major bacterial groups, gram-positive and gram-negative or any antibiotic that acts against a wide range of disease-causing bacteria. They are lifesaving when no other antibiotic therapy is working.
They do come, however with their own set of whole set of detrimental, long lasting health effects. Some of these include resistance to pathogens, altered gut microbiota and immune system dysfunction. This is especially detrimental in young children. Broad spectrum antibiotics can alter gut microbiota which in turn will disrupt and affect immune function and growth of the child.
Promising research to fight antibiotic resistance
A protein in antibiotic resistant bacteria called DsbA helps fold resistance proteins into the right shapes to neutralize antibiotics. This was discovered by researchers, including experts from Imperial College London, led by Dr Despoina Mavridou assistant professor in Molecular Biosciences at the University of Texas at Austin. By disrupting the DBsA protein the team was successful in neutralizing the antibiotic resistant protein. In addition the pathogen was more sensitive to common antibiotics. As of this writing, research has been limited to outside the human body. The team now plans on finding an inhibitor that can be safely used in humans providing the same effect.
How to prevent AMR
Until research can successfully develop therapies for AMR, staying healthy and using antibiotics only when necessary are our options. Also, avoid crowds during outbreaks. And if sick, stay home!
The most effective way to prevent AMR is to boost immune system through:
- Quality sleep- Sleep is when the body actively heals and restores health. Practice sleep hygiene
- Exercise- At least 30 minutes several times a week of active walking or other form of exercise can help boost immune system, regulate mood and decrease appetite
- Avoid sugar-Sugar and refined carbohydrates help feed pathogenic bacteria
- Vitamin D (with k2)- Vitamin D supports a strong immune system. Talk with your healthcare provider about vitamin D supplementation and checking vitamin D levels to make sure you are reaching optimum vitamin D levels
- Avoid and manage stress- Deep breathing exercises can help when unable to avoid stressful situations.
- Practice personal hygiene- wash hands after going to store, before eating, and any time your are exposed to anyone who is ill.
- Brooke Lounsbury, RN
Medical Content Writer
Lifesaving Medications
Recent Posts
Keeping you informed and safe.
Practice an Attitude of Gratitude for Even More Resiliency
Does Your Child Play Sports? Know the Signs of a Concussion
A concussion is a type of traumatic brain injury—or TBI—caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull,...
Fight Colds and Flu Symptoms with These Natural Treatments
Along with over-the-counter medications to relieve the symptoms of colds and flu, there are some effective, research-based remedies to reduce cold and flu symptoms, and in some cases help prevent the onset of colds and flu. Before modern medicine, our ancestors had to...